Reasons Why Medical Practices are Losing Money:
- Claim denial frequency higher than 4%
- Initial claim approval rate falling short of 98%
- Overall collection rate dropping below 97%
- More than 12% of accounts receivable aged over 90 days
- Poor communication affecting workflow.
- Irregular tracking and reporting of essential performance metrics
- Escalating administrative expenses reducing profitability
- Misalignment between staff roles and their skills or responsibilities.
- Not having Right people for the Right Job
For Peak Efficiency:
Our Client Base
RcmTree provides comprehensive medical billing and revenue cycle management services to a wide range of healthcare providers. We work with clients of all sizes from solo practitioners facing the challenges of a complex healthcare system to large medical groups and healthcare organizations with high-volume operations.
Our Services
Smarter and Scalable Solutions
RcmTree All in one Solution
Revenue Cycle Management
Medical Coding
Credentialing, Enrollment & Contracting
Eligibility Verification & Prior Authorization
Out-of-Network Negotiations & IDR/TDI Support
Virtual Assistant & Administrative Services
RcmTree Specialities
RcmTree partners with healthcare providers nationwide to optimize financial success. Our expert billing and practice management teams offer end-to-end solutions, helping private practices of all sizes improve revenue and focus on patient care
Ambulatory Surgery
Mental Health
Pain Management
Allergy & Immunology
Pathology
Internal Medicine
Urology
Neurology
Cardiology
Ophthalmology
Gastroenterology
Dermatology
Urgent Care
Orthopedic
Wound Care
Emergency Rooms
Ear, Nose & Throat
FQHC
Infectious Disease
Nephrology
Oncology
Nursing Homes
Pulmonary
Our process
Our Medical Billing Process
At RcmTree, we ensure a smooth and efficient journey from patient care to payment. Here’s how our process works:
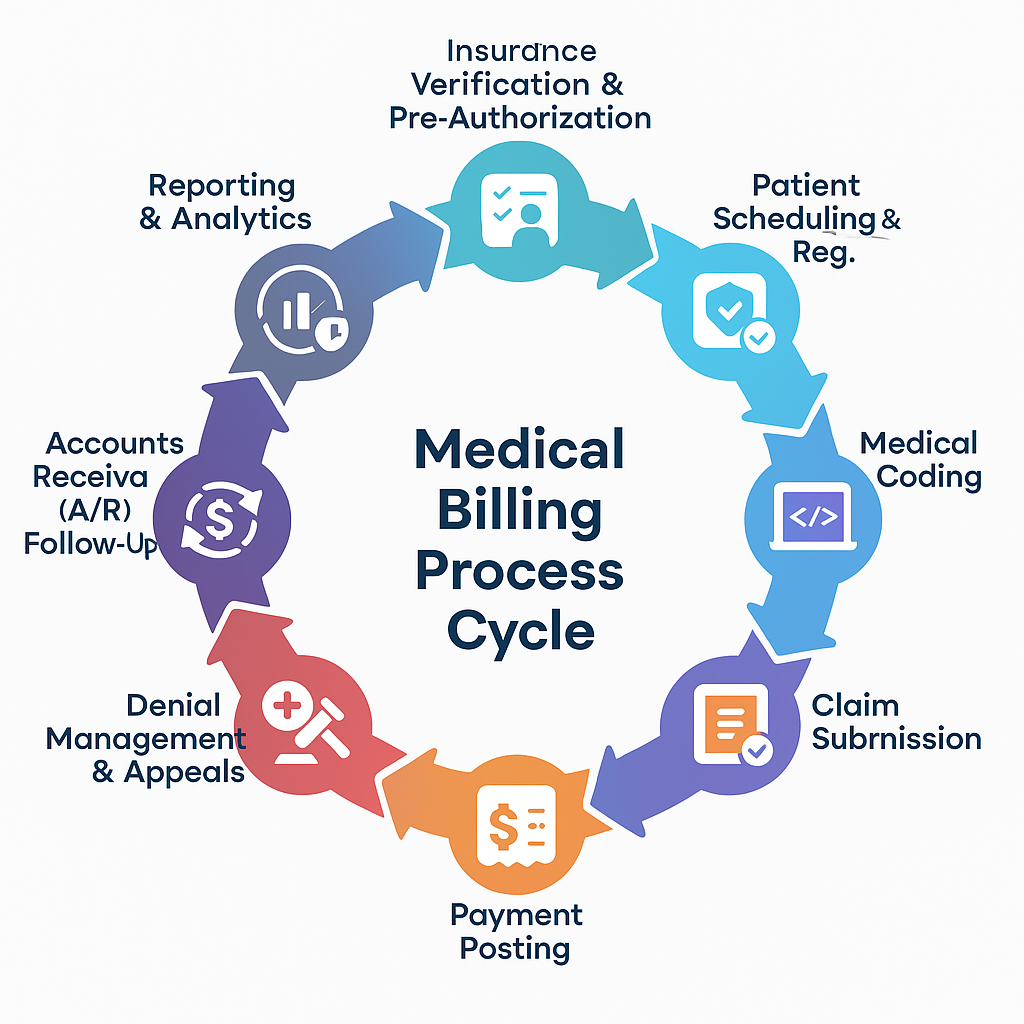
We collect essential patient demographics, insurance, and contact details to start the billing journey accurately.
Our expert coders assign precise codes to diagnoses and services, critical for accurate insurance billing.
We meticulously prepare claims, detailing patient, insurance, and coded services for submission.
Claims are electronically submitted to insurance companies, ensuring rapid processing.
Insurers review claims for accuracy and sufficiency, determining payment based on coverage.
Accepted claims trigger payment to you; denied claims are promptly appealed or resubmitted by our team.
Patients are responsible for co-payments, deductibles, and any amounts not covered by their insurance. We handle patient billing and diligently work to recover all outstanding balances.
